Study findings offer new insights into long-term outlook for ACL surgery patients

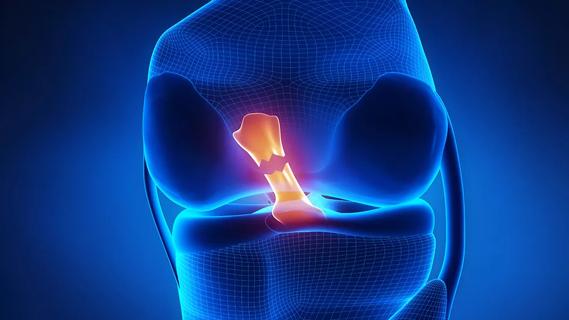
The conventional wisdom regarding patients who have had reconstructive surgery of the anterior cruciate ligament (ACL) has always been that the surgery leaves them with less overall function in that leg, and that diminished muscle function likely influences long-term outcomes. However, in a new study in the journal Clinical Biomechanics, Jillian Beveridge, PhD, of the Department of Biomedical Engineering, and colleagues have found that muscle coordination in patients who had ACL reconstructive surgery was similar to that of uninjured control subjects 10 years after the surgery.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Following surgery, patients tend to adopt muscle compensation strategies that serve to protect the knee. Up to this point, previous research suggested this to be true even several years after the surgery. To Dr. Beveridge’s knowledge, this is the first study to examine neuromuscular function so long after ACL surgery. The original aim of the study was to identify muscle activity patterns that may place patients at greater risk of developing degenerative joint changes associated with osteoarthritis.
“Consistent with what others in the field have reported, we anticipated that patients who had ACL surgery would have different muscle function in their reconstructed knee versus their healthy knee or the knee of a healthy uninjured person,” said Dr. Beveridge, “but, interestingly, that’s not what we found.”
Dr. Beveridge and her team studied 18 subjects (nine who had ACL surgery and nine healthy control subjects) as they performed a one-legged “hop test”—jumping and landing on the same leg—comparing how far the patients could hop and land without taking a second step to maintain their balance.
The researchers assessed neuromuscular function by attaching electrodes that measure electrical activity to various parts of the subjects’ lower limbs (thigh, between the knee and ankle, and foot), helping them to determine when subjects engaged their leg muscles as a compensatory or protective measure.
The researchers found that patients who had ACL surgery hopped slightly shorter distances, but—surprisingly—had nearly identical neuromuscular function as the control subjects. The main difference was that surgical patients had a delayed response in engaging their hamstring muscles for both legs.
The findings may have implications for ACL patients who are already at greater risk of re-injuring their knee or injuring their other knee. Given that the hamstrings normally protect the ACL from injury, a delay in hamstring activation may place the ACL at greater risk of injury. Dr. Beveridge noted that patients who have had an ACL injury and repair are at greater risk for osteoarthritis, but the current results showed that subjects had symmetrical muscle activity and coordination in both legs even 10 years after surgery.
“Given our surprising findings, we aren’t sure how muscle function relates to osteoarthritis risk, but the delayed hamstring activity we observed in both limbs may mean that those patients were at greater risk of ACL injury to begin with,” she said. She added that the results of this study and assessment of cartilage health may yet provide a greater understanding of the risk of osteoarthritis in these patients, but further study is needed.
She also noted that, because of the similar electromyography measurements between surgical patients and controls, other factors, such as the injury itself, the surgery or the rehabilitation after the surgery, may have more direct bearing on the long-term outlook for ACL surgery patients.
This study was supported by the National Institutes of Health, the Lucy Lippitt Endowment and the RIH Orthopaedic Foundation.
This story was adapted from LRI News.
Study reports zero infections in nearly 300 patients

How to diagnose and treat crystalline arthropathy after knee replacement

Study finds that fracture and infection are rare

Reduced narcotic use is the latest on the list of robotic surgery advantages

Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions

How it actually compares to posterior and lateral approaches

When procedure is performed by high-volume surgeons, outcomes are comparable to total knee replacement
Clot substitute helps rejoin the stumps of a torn ligament