Continuity of care to the fullest

Disease management for patients with COPD requires a holistic approach, especially for those patients with higher symptom burden and healthcare utilization. Through the Bundled Payment for Care Improvement Advanced (BPCIA) program offered through the Centers for Medicare and Medicaid Innovation, Cleveland Clinic is able to provide in-home skilled visits for patients that traditionally have not been able to receive follow-up care.
Debasis Sahoo, MD, Quality Officer, COPD Champion and pulmonologist at Marymount Hospital, introduced the concept of providing in-home respiratory therapy and pharmacy support to COPD patients post-discharge. As a result, Cleveland Clinic Center for Connected Care and COPD Physician Champions created an innovative in-home multidisciplinary disease management program.
“At Fairview Hospital, a care continuum model based on stakeholders’ feedback aimed to eliminate the siloed approach of transitions of care,” says Cleveland Clinic pulmonologist, Anu Suri, MD. “This is the result of long hours, multiple brainstorming sessions, flexing to the needs-based on data-driven strategy and a team of teams approach. The current model based on our teams’ vision has led to an improvement in patient outcomes, specifically in the areas of avoidable re-hospitalizations.”
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our goal is to deliver a comprehensive, evidence-based, coordinated plan of care to support our COPD patients, both during their hospitalization and also to support patients’ individual needs post-discharge,” says Dr. Suri. “We have learned that the immediate post-hospitalization period is one of the most vulnerable times for our patients. We created a team-based care and education model which keeps frequent touchpoints for the 90 days post-anchor admission. This helps identify early signs of an exacerbation that could be treated in a timely and effective manner.”
Along with a COPD Champion like Dr. Suri, specialists from Cleveland Clinic’s Outpatient Pharmacy and Home Respiratory Program collaborate to provide medication and disease-specific education. This ensures patients with COPD understand how to care for themselves at home and feel empowered to take charge of their health, yet, cognizant of when to call for help.
“Within five days of discharge, a member of our respiratory therapy team visits the patient’s home for an assessment,” says Mary Mertens, RRT, a Clinical Manager at Cleveland Clinic. Respiratory therapists work to keep patients connected to high-quality care as they transition to home. Through this program, the therapist becomes the patient’s trusted COPD resource at home, which empowers patients to gain confidence in managing their disease and understanding signs and symptoms of exacerbation.
The program begins with two in-home visits in the week following hospital discharge. Over the 12-week program, the respiratory therapists provide disease-specific education and clinical assessment and review their home for any environmental concerns that may contribute to exacerbations of the disease. Therapists also confirm the patient has the prescribed respiratory medications and ensure that the patients are using their inhalers and nebulizer medications correctly.
If at any time during the in-home visit the patient demonstrates any signs of deterioration, the therapist contacts the Physician Champion. This timely and effective communication leads to early intervention and has helped avoid unnecessary emergency department visits and re-hospitalization. Eventually, the weekly visits transition to virtual or telephone.
In addition to the in-home and virtual support of respiratory therapists, patients are also supported by outpatient pharmacists who help manage medication issues. Pharmacists identify gaps in a patient’s pharmaceutical therapy. Some of the examples include empowering the use of long and short-acting bronchodilators, researching the most cost-effective formulary products and helping patients better understand the rationale of using the prescribed medications.
Cleveland Clinic outpatient pharmacists check-in with patients by phone at day 15, 45 and 75 post-discharge. These calls ensure patients have all their prescribed medications, pharmaceutical therapy appropriate for their condition, can use the nebulizer or inhaler correctly, and if there are any issues with affordability.
If any gaps are identified, the pharmacist works with the patient’s COPD Physician Champion to update prescriptions and research patient assistance programs to help mitigate affordability issues. Noncompliance with medications due to cost constraints is a major challenge with the COPD patient population.
“Medication management might not be addressed while the patient is in the Emergency Department,” says Anthony Kitchen, RPh, Ambulatory Pharmacy Manager at Fairview Hospital. “That’s a hard place for them to retain information.”
“At the beginning of the pandemic, patients with COPD were hesitant to seek care even if they were struggling or experiencing disease flare-up,” says Dr. Suri, noting that mindset has translated to poor outcomes. Through the implementation of universal mask use, safe distancing and hand hygiene, patients have again been seeking help in healthcare settings. Cleveland Clinic is committed to providing care to patients in whichever setting they feel safest, whether that’s virtual, phone or in-person visits.

A review of conservative, pressure-based and surgical treatments for OSA

A review of IDSA and NIH guidelines

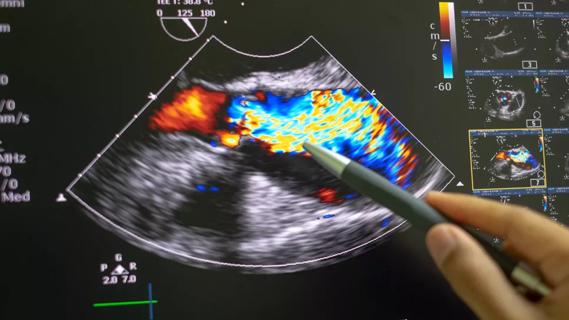
Volatile organic compounds have potential in heart failure diagnostics

Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients

New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality