Essentials of the case and implications for future transplants
When Cleveland Clinic announced last summer that it had performed its third face transplant — and first total face transplant — in May 2017, it may have seemed like a self-limited event. Now that the transplant recipient, Katie Stubblefield, and her family are comfortable sharing details of her case, as profiled in depth in an online National Geographic report, it’s becoming clear just how extensive a clinical journey it has been for the patient and her large team of managing clinicians.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The transplant, which has left Katie faring well through 15 months of follow-up, is distinctive in a number of respects, as detailed below.
Patient age. Katie was 21 when she received her face transplant, making her the world’s youngest face transplant recipient reported to date. The transplant was pursued to address the effects of severe facial trauma from a gunshot wound in March 2014, when Katie was 18.
Complexity. Katie’s transplant was the most extensive and complex of the three face transplants performed at Cleveland Clinic so far and among the most complex of the approximately 40 face transplants reported worldwide.
The 31-hour surgery involved replacing effectively 100 percent of Katie’s facial tissue, including scalp, forehead, upper and lower eyelids, eye sockets, nose, upper cheeks, upper jaw and half of lower jaw, upper and lower teeth, partial facial nerves, and facial muscles and skin.
The surgical team included nine plastic surgeons in the OR (plus resident staff) along with two consulting surgeons extensively involved in surgical planning. That’s in addition to a small army of nonsurgeon physicians from multiple specialties and other clinicians — psychologists, physical and occupational therapists, speech therapists, specialized nurses, dentists, pharmacists, social workers and others — involved in Katie’s full spectrum of care before and after transplantation. That care was especially notable due to the extreme nature of her facial trauma (detailed below) and the trauma-related destruction of part of her pituitary gland, which gave rise to endocrinopathies and related complications.
Advertisement
The result is that now all of Katie’s skin from the mid scalp down to the neckline is from her donor, as is a significant portion of her facial bone structure, including her orbital floors, her upper jaw and approximately two-thirds of her lower jaw.
“Despite the extensive replacement of skin and bone, the most complex aspect was the vascularity of the lower and upper jaws,” notes Francis (Frank) Papay, MD, who led the transplant surgery team along with Brian Gastman, MD, and consulting surgeon Maria Siemionow, MD, PhD. “The complexity of dissecting out the donor’s vessels to allow the vascularity to improve the blood supply to the lower and upper jaws was relatively new to us. And in this case we included, for the first time, the technically challenging internal maxillary artery to increase the robustness of the blood supply.”
“The vascularity of the tissue was the biggest issue for us as reconstructive plastic surgeons,” adds Dr. Gastman, citing the need to rapidly connect a multiplicity of donor and recipient vessels while the composite graft had no blood supply and the clock was ticking. Both he and Dr. Papay are board-certified in plastic surgery and head and neck surgery. Dr. Siemionow, who is now with the University of Illinois at Chicago, is former director of Cleveland Clinic’s Department of Plastic Surgery Research and is director of the grant from the U.S. Department of Defense that supported the transplant (detailed in this earlier Consult QD post). She served as an adviser throughout the case.
Advertisement
Further adding to the complexity of Katie’s case is the fact that her facial trauma was self-inflicted from a gunshot in a suicide attempt (as discussed in the National Geographic report), which required particularly extensive psychiatric and social evaluation of Katie and her family to confirm she was fully committed to living and had the extraordinary support system needed before and after the transplant.
Degree of preparation and planning. When Katie was transferred to Cleveland Clinic from an outside hospital six weeks after her trauma, one of her family’s objectives was evaluation for possible face transplant. Three years passed before she was ready for the transplant and an appropriate donor was found, which gave the team an abundance of time to prepare.
“Katie was my patient from her arrival here,” says Dr. Gastman. “We knew early on that she seemed to be a good candidate for eventual face transplantation, so we pursued a series of facial reconstruction operations to prepare for that and get her functioning better. We learned from our prior face transplants the importance of preserving her vessels and nerves as much as possible during these procedures, recognizing we would likely need them for a transplant.”
“We planned and planned and planned, and then we planned some more,” says Dr. Papay. For months, members of the surgical team performed multiple mock surgeries in Cleveland Clinic’s cadaver lab and by using the Microsoft HoloLens augmented reality platform.
Dr. Papay says both of those resources proved priceless. “The cadaver lab is probably the most valuable resource we have as plastic surgeons, allowing us to learn and relearn the microanatomic intricacies of the entire body,” he notes. “And the HoloLens — together with standard stereolithographic [3D-printed] models, which we also used for our prior face transplants — allowed us to visualize Katie’s anatomy in 3D and plan and practice the surgery in a way we’d never been able to before.”
Advertisement
The planning and practice extended to multiple members of Katie’s surgical and medical teams. “We built multiple redundancies into our process, to ensure we’d be ready whenever the right donor opportunity arose, regardless of who was in town,” Dr. Gastman explains.
Use of HoloLens. The above-noted use of the Microsoft HoloLens is the first known deployment of this or similar augmented reality technology in planning a face transplant, according to Dr. Papay. It resulted from a year of collaboration between the transplant team and the lab of Karl West, MS, in Cleveland Clinic’s Lerner Research Institute, which had been working on HoloLens applications in vascular surgery and other areas. “We were able to take Katie’s CT data set before the transplant and extrapolate out 3D representations of her skull, bony structures and — most important — vascular structures to allow the surgeons to see them in relation to each other,” West explains.
“It was like having X-ray vision,” Dr. Papay observes.
Once a donor was identified, West’s team scrambled to generate, within hours, a similar 3D holographic display of the donor’s anatomy for the surgeons to superimpose onto Katie’s face right before and during the transplant surgery. For more on the use of HoloLens in the transplant, see this related Consult QD post.
Avoidance of a palatal obturator. Insights from the surgical team’s prior face transplants helped them dissect blood vessels far in the back of Katie’s throat, near where the soft palate meets the hard palate. The team has hypothesized that this may be a watershed area for blood supply and thus critical to healing and avoidance of a fistula and the resulting need for a palatal obturator. “Katie is one of the first face transplant recipients to not have a hole in the palate area,” says Dr. Papay. “That’s a testament to our extensive anatomic studies in the cadaver lab to practice dissecting the tiny blood vessels as far back as we could.”
Advertisement
When Katie arrived at Cleveland Clinic in May 2014, six weeks after her trauma, she was “in dire need of very advanced craniofacial care,” Dr. Gastman says. Despite several initial surgeries at outside hospitals, she was contending with multiple functional issues, including loss of vision and loss of the ability to speak, breathe through her nose, swallow food, chew and move her tongue. Her intracranial injuries had caused traumatic brain injury and led to memory deficits and limb spasticity. Beyond her loss of vision, she had major dystopia of the eyes. Hormonal disorders resulted from the damage to her pituitary, and she had significant infection of skull base tissues. She was also grappling with the clear psychosocial effects of her trauma and disfigurement.
She soon began a series of more than a dozen surgeries at Cleveland Clinic to address functional or medical issues and prepare her for possible face transplantation. Two were major reconstructions using autologous tissue from the leg. The first rebuilt the top of the mouth and the nasal airway and sealed off the brain from the infected skull base tissue before evacuation of the colonized tissue. The second major reconstruction rebuilt part of the missing lower jaw and lips. For the latter operation, Dr. Gastman led an effort to develop a custom titanium plate based on a 3D CT of Katie’s older sister, whom Katie resembled before her trauma.
Other important surgical milestones included collaboration with neurosurgery to place a customized cranial implant (based on Katie’s contralateral normal skull) to provide durable cranial coverage, as well as distraction osteogenesis to widen her periorbital bone to optimize it for transplantation.
“These were challenging reconstructions because we had few landmarks to build from, given the extent of her trauma,” Dr. Gastman explains. “But they allowed us to reduce the length and complexity of the ultimate transplant operation.”
After some of the initial surgeries, Katie began outpatient rehabilitation for physical, occupational and speech therapy. Her spasticity resolved and her functional abilities improved, including her walking, speech and swallowing.
Nevertheless, obstacles arose along the way, such an acute deep vein thrombosis early in the course of her surgeries, the emergence of generalized tonic-clonic seizures (likely related to a drop in sodium) and development of Clostridium difficile infection. “These developments underscore the necessity of comprehensive multidisciplinary excellence in the management of a case like this,” notes Dr. Papay.
By the fall of 2015, Katie began multidisciplinary evaluation for a possible face transplant, for which she was listed in March 2016.
The transplant itself took place a little more than a year later, as detailed on Consult QD soon thereafter and in new posts related to the crux of the operation and the team dynamics of the intraoperative decision-making involved.

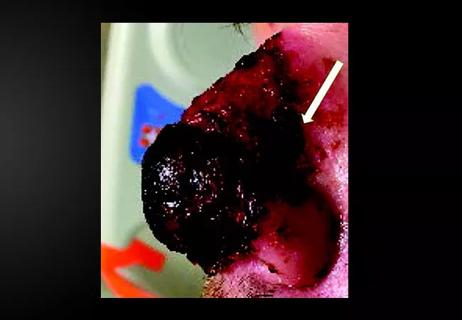
Katie in March 2015, after some but not all of her pre-transplant reconstructive surgeries, and in August 2018, 15 months after her total face transplant.
In the 15 months since her transplant, Katie has had a few revision surgeries to achieve specific adjustments, such as advancing the base of her tongue, advancing the orbital wall and adjusting her lower jaw for better alignment with the upper jaw. Dr. Gastman doesn’t expect many additional revisions, but Katie will soon receive a prosthesis from a prosthodontist to elevate her soft palate to help reduce her vocal hypernasality.
She is healthy and has had few rejection episodes, including no recent episodes and the fewest of any of Cleveland Clinic’s three face transplant patients to date, Dr. Papay notes. He adds that although her young age is in her favor, the risk of rejection will remain the primary concern for Katie indefinitely.
Functionally, she has improved considerably since the transplant in her speaking and articulation, her swallowing and ability to eat orally, her ability to show emotion with her face (“she’s starting to be able to smile,” Dr. Gastman notes) and her ability close her eyelids. “We don’t expect her to stop improving,” Dr. Papay says.
Both surgeons attest to a marked improvement in Katie’s psyche while underscoring that she is still just starting on a long road toward gaining more independence and ultimately finding a place again in the broader world. They expect that will take additional years of rehabilitation and continued strong family support, but they see real potential for her to achieve her goal of becoming a spokesperson for suicide prevention among young people.
Beyond the gains for Katie, Drs. Papay and Gastman identify a number of gains from this case for the face transplantation field as a whole, including the team’s pioneering use of HoloLens augmented reality and the novel inclusion of the internal maxillary artery in the mix of vessels dissected.
“There are things we learn from each face transplant that we never knew before,” Dr. Papay says. “A good example is the recovery of facial sensation. In our first two patients, there were areas where we didn’t transplant sensory nerves, yet the patients eventually recovered much of their facial sensation. We hypothesize that recruitment of the surrounding nerves might have filled in those areas, but we’re not sure. So we tried to incorporate sensory nerves in Katie’s transplant as much as possible, and we will be monitoring eventual return of sensation.”
Meanwhile he and his Cleveland Clinic colleagues are pursuing a number of new frontiers in face transplantation, including:
An even bigger challenge may be finding a way for society to fund more face transplants. “We and others are showing that these are not one-off cases anymore and we can dramatically improve the lives of people with facial trauma that would have been inconceivable to treat a few decades ago,” says Dr. Gastman. “The medical community and government need to take on this question, because there are other Katies out there.”
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair