Resection is possible with multidisciplinary approach
A 35-year-old woman reported decreasing vision in her left eye. She had noticed difficulty focusing one year earlier, with 20/50 vision, and had been seen several times at an outside hospital.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
On presentation at Cleveland Clinic, her visual acuity was 20/400 OS with an afferent pupillary defect. The patient also had 3 mm of left proptosis and ptosis of the left upper eyelid.

Visual field before surgery

3 mm of left proptosis before surgery
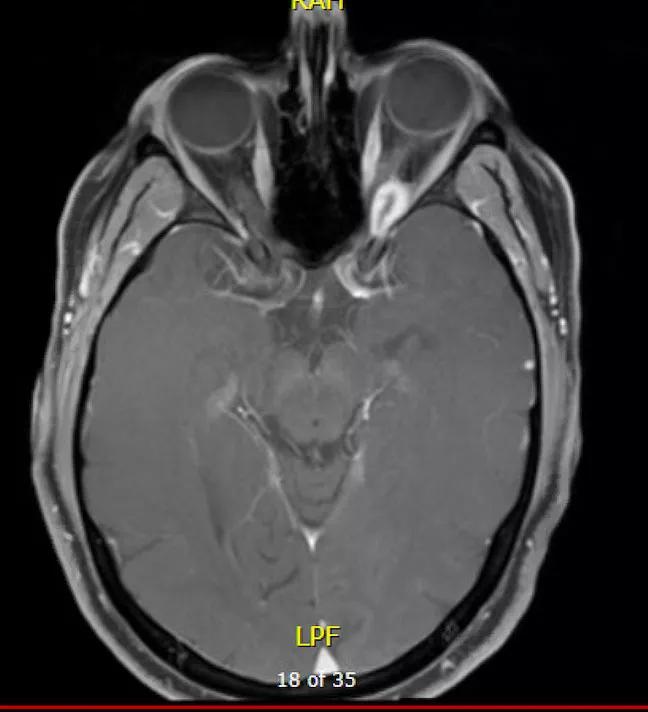
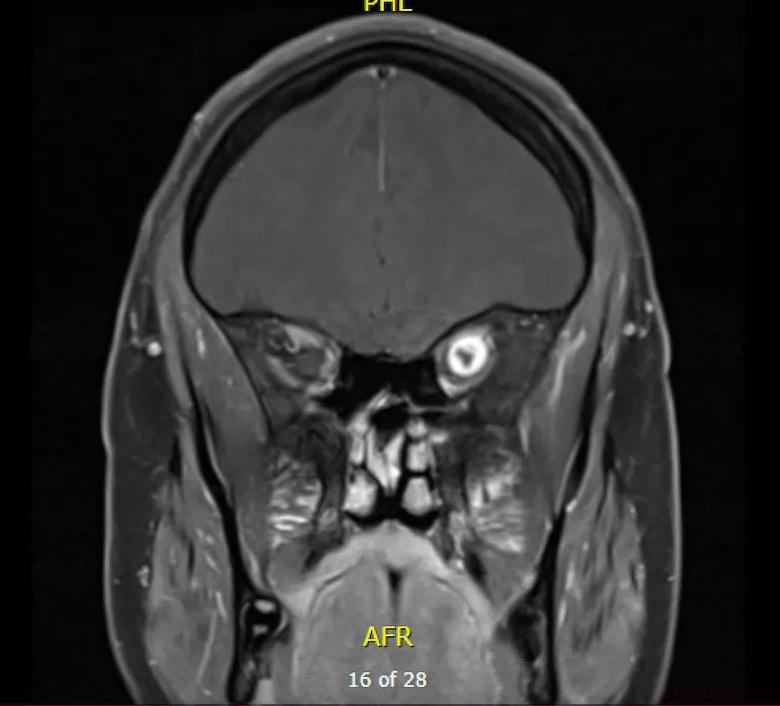
Magnetic resonance imaging (MRI) and computed tomography (CT) scans revealed an orbital apical tumor 1.6 x 0.8 cm.
Because the patient’s outside ophthalmologist believed the tumor to be unresectable, the patient had been referred to Cleveland Clinic for radiation therapy. However, because radiation therapy to the compact orbital area can cause permanent vision loss, nerve damage, and retinal and corneal changes — and doesn’t eliminate benign tumors — a multidisciplinary team at Cleveland Clinic took a fresh look at the case.
After reviewing all available treatment options, the team determined that with a collaboration of specialists the area could be accessible surgically and the tumor could be removed. Catherine Hwang, MD, an orbital specialist and oculofacial plastic surgeon in Cleveland Clinic’s Cole Eye Institute, worked with surgical experts in Cleveland Clinic’s Neurological Institute to formulate a plan and tailor an approach for the patient.
“The orbital apex is a high-risk area with high-risk real estate — including all the nerves, such as the optic nerve, and blood vessels that supply the eye and eye socket,” says Dr. Hwang. “The only way to access the tumor in order to perform the orbital dissection is with a neurosurgical approach. At Cleveland Clinic we have a multidisciplinary team with the skills to remove these difficult tumors.”
Because the tumor was superior and slightly lateral to the optic nerve, the neurosurgery team led by Varun Kshettry, MD, a skull base surgery specialist in Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center, performed a craniotomy with a superior lateral approach to the orbital apex.
“We needed access to the posterior orbit with enough space to visualize the entire orbital apex so we could dissect around the eye’s blood vessels and nerves,” says Dr. Hwang. “These structures that converge in the apex affect not just vision, but muscle movement of the eye and eyelid. Any surgery in the orbit can cause permanent vision loss, but surgery in the orbital apex increases that risk.”
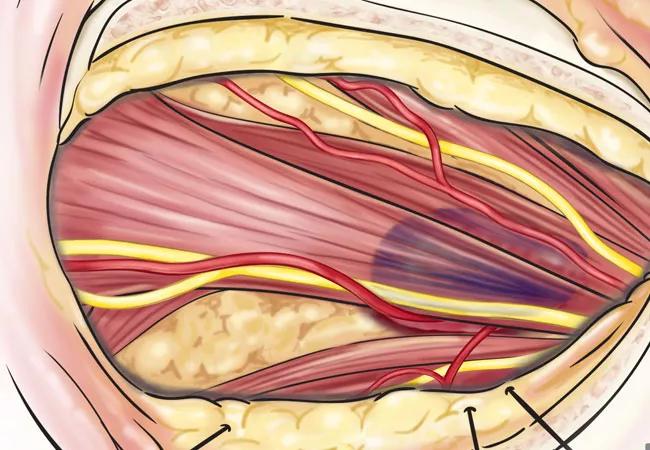
During the 5.5-hour procedure, Dr. Kshettry gained access to the tumor, and Dr. Hwang used an operating microscope to visualize the tumor in the back of the eye socket. She brought the tumor forward using a traction suture technique and then used microneurosurgical dissectors to free the tumor from its attachments.
Drs. Hwang and Kshettry removed the 1.6 x 0.9 x 0.5 cm tumor in one piece.

Following the resection, the orbit was reconstructed with collagen matrix and titanium plating to restore the patient’s appearance.
The patient was discharged from the hospital two days after surgery. On day 11 post-surgery, Dr. Hwang examined the patient during an office visit. The patient’s vision was 20/25, and she had no afferent pupillary defect, although ptosis was still evident and ocular movement was limited.
The patient remarked that she was extremely pleased with the rapid improvement in her vision.
Two months later, the patient was 20/20 with no afferent pupillary defect, no proptosis and full resolution of ptosis.

Visual field after surgery

Appearance restored after surgery
Orbital tumors may or may not cause vision problems. Benign tumors with no adverse effect on vision may not require resection, but rather can be monitored. Surgery in the orbital apex is always high risk, yet is possible for patients with troublesome symptoms such as double vision or vision loss.
“Any kind of orbital tumor should be referred to an orbital specialist so the patient can be evaluated and counseled on next steps,” says Dr. Hwang, a member of the American Society of Ophthalmic Plastic and Reconstructive Surgery.
Although most orbital tumors can be accessed via the orbital approach, some tumors need a multidisciplinary approach, she adds. Multidisciplinary teamwork in this case provided an excellent outcome for a patient with a deep orbital apical tumor.

Determining the right dose and injecting in the right muscle can be challenging
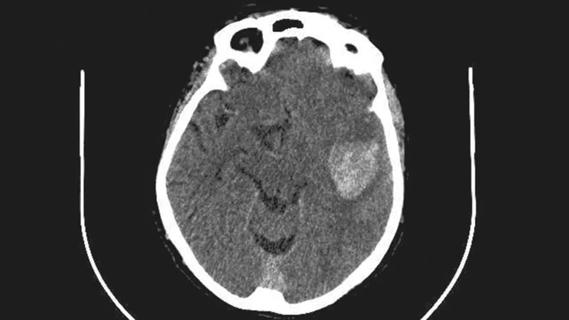
ENRICH trial marks a likely new era in ICH management
Study combines intracranial electrophysiology and SPECT to elucidate the role of hypoperfusion
New research sheds light on a potentially devastating condition that is reversible when properly managed

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond