Combined transepithelial PTK, CXL yields improvements

Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 24-year-old graduate student from the East Coast presented to the Cole Eye Institute for contact lens fitting. She reported having several years of increasing myopia and astigmatism with frequent spectacle and contact lens changes, and we made a diagnosis of keratoconus at that visit. She was concerned about her recent decrease in vision and reduced contact lens tolerance and was promptly referred to the Cornea and Refractive Surgery service.
Her best spectacle-corrected visual acuity was 20/25- in each eye with manifest refractive error of -3.75 + 4.25 x 005 OD and -4.75 + 1.25 x 095 OS. Scheimpflug tomography demonstrated predominantly central cones with co-localized anterior and posterior surface elevation and thinning (right eye shown in Figure 1). Working around her busy final exam schedule, we decided to proceed with corneal crosslinking (CXL) in the right eye to address the disease progression before further loss of spectacle-corrected vision occurred.
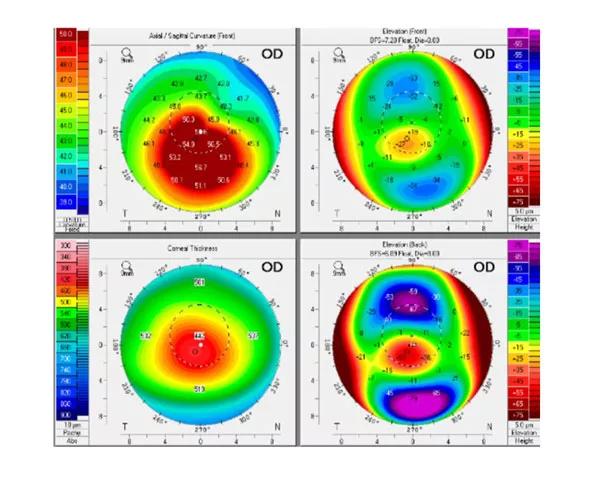
Figure 1
Research conducted at the Cole Eye Institute’s Ocular Biomechanics and Imaging Lab has demonstrated through patient-specific computational modeling how progressive localized weakening of the corneal stroma can occur insidiously in keratoconus with little evidence of topographic change until advanced weakening has occurred (Figure 2). If left unchecked, this weakening will lead to exponential increases in corneal steepness and asymmetry and, as a result, potentially irreversible degradation of corneal optics and retinal image quality.
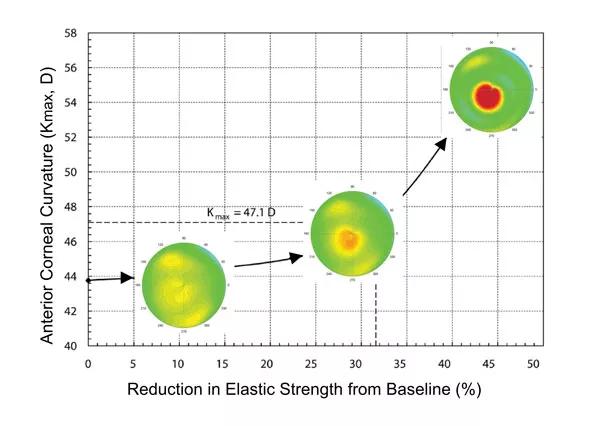
Figure 2
CXL is a major advance for stabilization of keratoconus. But in this young patient who had already lost lines of vision from progression, we sought to customize her treatment in a way that would offer a greater chance of visual improvement while also halting disease progression.
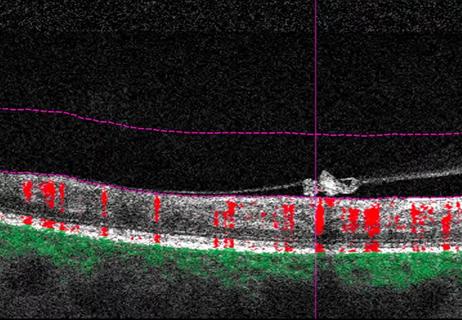
To this end, spectral-domain optical coherence tomography mapping of her corneal epithelial thickness profile was obtained. As illustrated in Figure 3, the epithelium was much thinner over the topographic cone (as thin as 39 µm) than in areas distal to the cone (up to 54 µm).
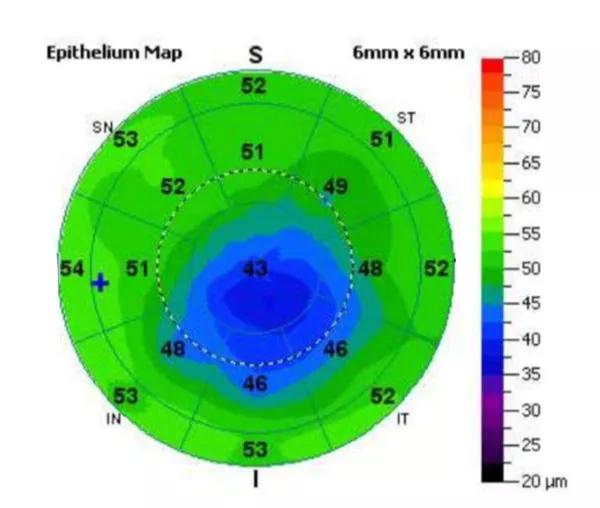
Figure 3
I made a surgical plan to use an excimer laser in phototherapeutic keratectomy (PTK) mode to produce a transepithelial ablation of 50 µm in depth. By leveraging the differential epithelial thickness, this approach was expected to produce a modest, selective 10 µm ablation of anterior stroma in the region of greatest stromal curvature and elevation, resulting in a targeted flattening effect. The remaining peripheral epithelium was then debrided manually to expose a 9 mm zone for the standard epithelium-off CXL protocol using riboflavin eye drops and UV light.
Three months after combined transepithelial PTK and CXL, the patient reported that her vision was much improved. Her manifest refraction had improved from -3.75 + 4.25 x 005 to -2.50 + 0.75 x 019 and she was able to read the 20/20 line in spectacles for the first time in years. A 2.5 D reduction in corneal steepness was seen on the interval subtraction map (Figure 4). She was able to discontinue specialty contact lenses and return to toric soft lenses, and there has been no evidence of disease progression over the subsequent year.
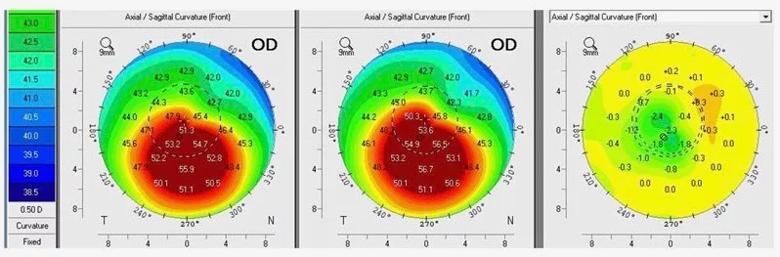
Figure 4
In this case, careful consideration of corneal structure and advanced imaging informed the approach to treatment and allowed us to leverage keratorefractive surgical techniques for more optimal treatment of the patient’s visual disorder.

Study highlights the value of quantitative ultra-widefield angiography

Switching medications may decrease treatment burden and macular fluid

Interventions abound for active and stable phases of TED

Corneal imaging and interpretation play a major role

Effect of low-dose atropine and dual-focus contact lenses is unknown in patients with comorbid eye conditions

How to screen for and manage treatment-triggered uveitis

Minimally invasive surgery is effective for uveitic and steroid-induced glaucoma too
Why retina specialists should get comfortable with this imaging tool